Wernicke-Korsakoff Syndrome, a debilitating neurological disorder, emerges primarily as a consequence of chronic vitamin B1 (thiamin) deficiency. The pivotal role of thiamin in overall brain function lends to its importance in our bodies. Our exploration begins with understanding the biochemical basis of this syndrome, delving deep into the intricacies of energy metabolism, thiamin transport, and the neurological damage ensuing from thiamin deficiency. As we describe the clinical presentation of the syndrome, enabling detection of its specific signs such as cognitive impairment, memory loss, and motor dysfunction becomes possible. Examining the risk factors, we shed light on the major contributors leading to this syndrome, highlighting the role played by chronic alcoholism, malnutrition, and certain genetic predispositions, which can all result in thiamin deficiency. To manage the disorder effectively, a clear understanding of its diagnostic and treatment approaches, alongside potential preventative measures, is crucial.
Table of Contents
The Biochemical Basis of Wernicke-Korsakoff Syndrome
Cellular Mechanics Behind Wernicke-Korsakoff Syndrome: A Crossroads of Thiamine and Neurological Dysfunction
Wernicke-Korsakoff syndrome (WKS), an often misunderstood neurological disorder, stems from one’s prolonged consumption of alcohol. It gives life to an intricate web of cellular processes disrupted by alcohol-induced thiamine (vitamin B1) deficiencies. At the heart of this unwelcome predicament lies thiamine, the critical nutrient whose scarcity plunges the human neural network into chaos.
Thiamine’s role as both an enabler and catalyst within cellular metabolism is pivotal. It takes up the responsibility of coenzyme in glucose metabolic pathways, thereby producing Adenosine Triphosphate (ATP) – the power source of every cellular function. Therefore, a subtraction in thiamine sends a ripple effect through the entire cellular metabolism framework.
Unlike most vitamins, thiamine does not accumulate in the body, meaning levels are vacuumed very swiftly by active metabolism, especially during alcohol consumption. Alcohol alters the integrity of the intestinal barrier, obstructs thiamine absorption, impedes thiamine utilization in cells, and speeds up renal excretion. The resulting thiamine scarcity directly impairs glucose metabolism.
Counterintuitive as it may seem, this metabolic impasse signals cells to switch to an alternate pathway: anaerobic metabolism. Unfortunately, this is an energy-expensive process, leading to the overproduction of lactic acid and resultant acidosis. As such, cells are thrust onto the brink of respiratory failure.
Simultaneously, thiamine lack adversely impacts neurotransmitter synthesis and myelin maintenance. Neurons become metabolically ‘starved,’ leading to cellular damage, axonal degradation, and myelin disruption, which ultimately brings on a whole host of detrimental neurological signs and symptoms.
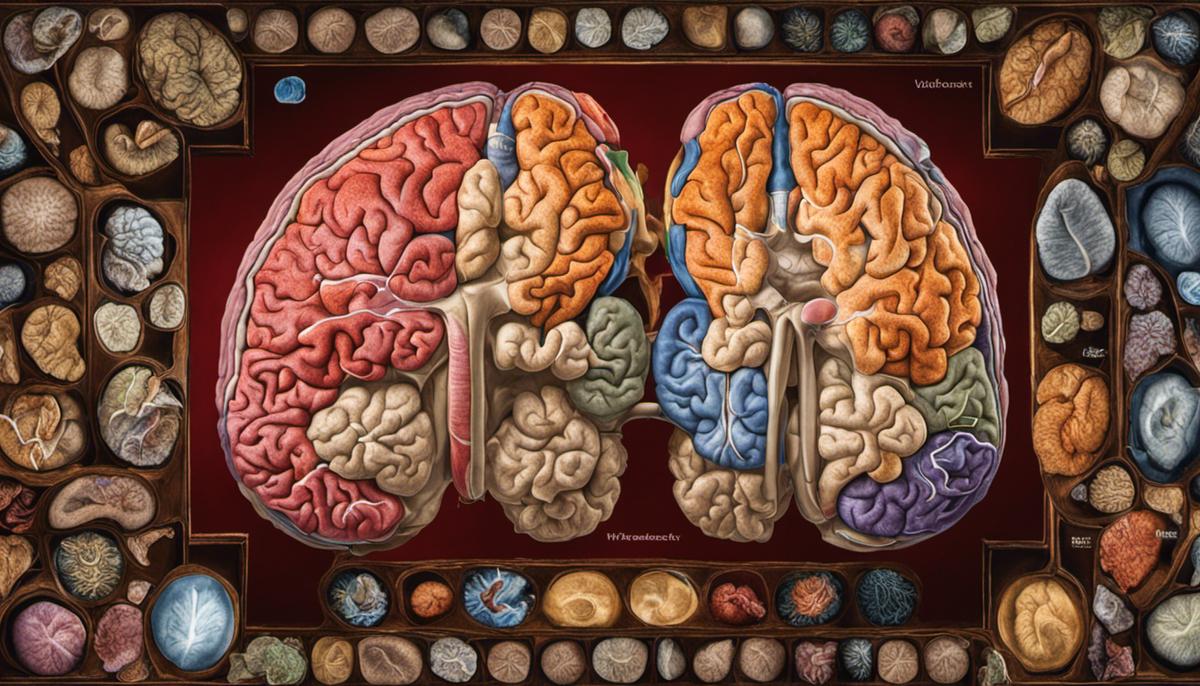
The brain’s regions most affected are the mammillary bodies and the cerebral cortex. Here, the cellular damage subverts normal functioning, unbalancing the regulation of memory, motor control, and executive function, hallmark characteristics of WKS.
The thiamine deficiency-induced oxidative stress further compounds the brain injury. It hampers neuronal function and integrity, leading to neuronal death and overall brain atrophy. Besides, a scarcity of thiamine disrupts the blood-brain barrier solution equilibrium, causing vasogenic edema and resultant cerebral hypoxia.
In essence, Wernicke-Korsakoff Syndrome represents a potent reminder of thiamine’s indispensable influence on cellular metabolism, neurotransmission, and neuroprotection. The butterfly effect of thiamine deficiency within cells identifies several opportunities for intervention and underlines the vitally significant intersection of nutrition and neurological health.
The Clinical Presentation of Wernicke-Korsakoff Syndrome
Continuing from the elucidation of the pathophysiological intricacies associated with Wernicke-Korsakoff Syndrome (WKS), let us examine the clinical manifestation and progression of this neurological disorder. WKS is characterized by two separate but overlapping conditions – Wernicke’s encephalopathy and Korsakoff’s psychosis – which often coexist.
Wernicke’s encephalopathy is acute in nature and generally precedes Korsakoff’s psychosis in the progression of WKS. Its triad of symptoms includes ocular abnormalities (including nystagmus, or rapid, involuntary eye movement), ataxia (a coordination disorder impeding the ability to execute voluntary movements), and global confusion. These result from thiamine deficiency-induced impairments in the mammillary bodies and thalamus.
Yet, not every patient displays the full triad; only around 16% of cases present all three symptoms, adding an element of diagnostic complexity. Unchecked, the consequences can be dire: progression to irreversible Korsakoff psychosis, or approximately 20% of patients developing coma or death if untreated.
Korsakoff’s psychosis, characterized by anterograde and retrograde amnesia and confabulation, is a chronic manifestation of thiamine deficiency. Here, patients find it increasingly challenging to form new memories (anterograde amnesia) or recall past memories (retrograde amnesia), the origin of which can be traced back to damage in the dorsomedial thalamus. Moreover, the patients may “fill in” gaps in their memory by fabricating misinformation that they believe to be true (confabulation). Given the irreversible nature of Korsakoff’s psychosis, lifelong management of symptoms becomes integral.
Moreover, WKS can manifest in individuals as peripheral neuropathy, a condition that displays as muscle weakness and atrophy, diminished reflexes, and numbness or tingling in the extremities. This symptom underscores the peripheral nervous system’s susceptibility to thiamine deficiency and the ubiquitous role of thiamine across all neural structures.
Understanding the progression and evolution of symptoms and signs in WKS equips researchers, clinicians, and caregivers better to detect, diagnose, and manage this condition. Complementarily, getting to the root of the cause, i.e., thiamine’s deficiency, provides a promising point of intervention. Regular and adequate thiamine supplementation can halt the progression of Wernicke’s encephalopathy symptoms, providing evidence of thiamine’s therapeutic significance. Yet, Korsakoff’s psychosis remains irreversible once present. Therefore, the importance of prevention, early detection, and immediate intervention can hardly be overstated.
In the grand scheme of neuroscience and nutrition research, WKS serves as an exemplar of neurological disorders caused by nutritional deficiencies and accentuates nutrition’s role as a foundation for neural health and function. As each piece of the puzzle fits together, it leads us one step closer to a holistic understanding of the interaction between nutrition and the nervous system, guiding us towards a future where neurological disorders can be more effectively understood, prevented, and treated.

Risk Factors and Causes of Wernicke-Korsakoff Syndrome
Building upon the extensive look into Wernicke-Korsakoff Syndrome (WKS) and its highly intricate pathophysiology, it is essential to delve into the risk factors and primary causes that significantly contribute to the onset of this debilitating syndrome. Without grasping these underpinnings, the medical community’s understanding of this syndrome would be notably incomplete and our capacity to intervene meaningfully hampered.
While thiamine deficiency acts as the central catalyst, repeated and chronic alcohol misuse undoubtedly veins out as the leading risk factor associated with WKS. It is imperative to comprehend that alcohol misuse disturbs not merely the absorption of thiamine but also disrupts its storage and activation. Such disruption precipitates serious biochemical implications that pave the way to WKS.
However, while the shadow of alcohol misuse looms largest, it is not the sole risk factor in the picture. Gastric disorders, particularly those necessitating surgical intervention, such as gastrectomy and gastric bypass surgery, also emerge as significant risk factors. The alterations these surgical procedures induce impair the gut’s ability to absorb thiamine efficiently. Additionally, malignant vomiting, linked to conditions such as hyperemesis gravidarum and carcinogenesis, can also trigger thiamine depletion due to the constant loss of vital nutrients.
Moreover, the onset of WKS has been associated with severe malnutrition, where nutrient deprivation extends beyond thiamine to include a widening spectrum of essential micro and macronutrients. In such a scenario, the collective nutrient paucity exacerbates the thiamine deficiency, pushing the nervous system into a perilous state of vulnerability.
Finally, this exploration would be remiss without acknowledging seemingly innocuous but nonetheless potentially detrimental factors like dieting, fasting, or existing eating disorders. These realities can inadvertently cultivate scenarios of nutrient depletion ripe for the onset of WKS.
It is important to underscore that the synergistic interplay between these risk factors escalates the likelihood of developing WKS. Therefore, medical practitioners must not only ensure thiamine replenishment but also address these underlying conditions to ensure a comprehensive therapeutic response.
With the magnitude of these risk factors and causes laid bare, the magnitude of WKS’s preventable nature is thrown into sharp relief. Raising awareness about these risk factors and promoting proactive measures of prevention, early detection, and immediate intervention will indubitably lead to reducing the incidence of this syndrome. Thus, seeking to understand these variables becomes central in our shared commitment to battling WKS effectively and preserving neural health and function as optimally as we strive to.
In conclusion, a more holistic understanding of the interaction between nutrition and the nervous system reveals complex intertwining narratives of vulnerability and resilience, a juncture where neuroscience and nutrition research must meet and meld to unfold brighter chapters of human health. This is not merely an academic exercise. It’s an essential path to carve out a future less burdened by the devastating implications of WKS and neurological disorders at large.

Current Diagnostic and Treatment Approaches for Wernicke-Korsakoff Syndrome
The diagnosis of Wernicke-Korsakoff Syndrome (WKS), a neurologic disorder typically resulting from severe thiamine (vitamin B1) deficiency, often proves to be a clinical challenge. It typically presents in long-term alcoholics and individuals coping with severe malnutrition. Given that the initial features are often subtle and inconsistent, it is often underdiagnosed, confounding the treatment regimen.
A vital tool in discerning a diagnosis appears in the form of magnetic resonance imaging (MRI), which provides a window into the brain’s structural integrity. MRI scans of WKS patients frequently reveal features consistent with symmetric thalamic, mammillary body, tectal, and periaqueductal lesions. However, it should be noted that MRI findings may be normal in up to one-third of patients with clinically diagnosed WKS, emphasizing the necessity for keen clinical acumen.
Another tangible diagnostic tool is the evaluation of blood thiamine concentrations, specifically thiamine pyrophosphate effect (TPPE). A TPPE of more than 15% is indicative of thiamine deficiency. However, a normal TPPE does not exclude the diagnosis, especially given the episodic nature of WKS.
Moving on to treatment strategies, the cornerstone remains early and aggressive thiamine replenishment. High-dose intravenous thiamine is strongly recommended in patients suspected of WKS until symptom resolution, given that oral thiamine replacement is often inadequate.
Notably, a report by the American Society of Addiction Medicine suggested the administration of parenteral thiamine 100 mg daily for three to five days in suspected cases. Ideally, this should be instituted even before confirmation of WKS if the clinical suspicion is high, as delay in treatment can lead to irreversible cognitive damage and substantial morbidity.
It’s essential to note that the symptoms of Wernicke’s encephalopathy and Korsakoff’s psychosis often overlap, with patients transitioning from one to the other. Complete resolution of symptoms following thiamine replacement is often seen in Wernicke’s encephalopathy, while perpetual cognitive impairment is the norm in Korsakoff’s psychosis.
Addressing underlying pathologies such as alcohol dependency and eating disorders is crucial to long-term management. Comprehensive rehabilitation programs, cognitive therapy, and abstinence from alcohol can delay disease progression and prevent relapse.
Wernicke-Korsakoff syndrome, a debilitating neurologic disorder, illustrates the critical interplay between nutrition and the nervous system, underlining the importance of preventative strategies. Robust diagnosis and prompt intervention can dramatically improve patient prognosis and quality of life. Only through a robust understanding of this interplay can we hope to make significant strides in combating disorders such as WKS.
Preventing Wernicke-Korsakoff Syndrome
Preventive strategies have a crucial role to play in stopping the initiation and advancement of Wernicke-Korsakoff Syndrome (WKS). Thorough awareness about the risk factors is a significant step in the prevention of WKS, specifically with regard to the harmful effects of chronic alcohol misuse, which is the most common risk factor lead to WKS. To sever the destructive chain of events, the potential consequences of alcohol misuse need to be effectively communicated to all strata of society, with particular emphasis on those at susceptible ages and communities where drinking is highly prevalent.
Apart from creating public awareness, personal healthcare habits and dietary precautions can be far-reaching. Proper diet, avoiding fasting or extreme dieting, and ensuring consumption of thiamine rich foods can bring about a substantial reduce in risk. It is necessary to understand that the body cannot store thiamine for extended periods. Hence, continuous consumption of thiamine-rich foods becomes crucial to sustain adequate levels of thiamine in the human body.
In clinical settings, patients presenting risk factors for thiamine deficiency should be handled with vigilance. Particularly, individuals with prolonged vomiting, gastrointestinal diseases, and those who underwent bariatric surgery, should be given competent nutritional support, usually involving supplementation of thiamine.
For individuals struggling with alcohol dependency, professional help to address the addiction issue is indispensable. Numerous evidence-based interventions are available including cognitive-behavioral therapies, motivational interviewing, and pharmacotherapies, which can help reduce alcohol intake, prevent relapse and hence mitigate the chance of developing WKS.
In all instances, medical professionals have a pivotal role to play. The initial signs of WKS can often be subtle and hence may be overlooked. A comprehensive understanding of the symptomatology, coupled with a high index of suspicion and immediate initiation of appropriate investigations is mandatory when patients at risk present with suggestive symptoms.
Remember, the advent of Wernicke’s encephalopathy, the precursor to Korsakoff’s psychosis, is an emergency. Immediate administration of parenteral thiamine can mitigate the damage and prevent the transition to Korsakoff’s psychosis, which is primarily irreversible. Hence, in the scenario of any doubt, medical professionals are urged to start thiamine administration considering the possible life-threatening effect of delay and the low-risk nature of thiamine administration.
Prevention of WKS not only relates to the wellbeing of individuals but expands to the societal level affecting the economy and public health. WKS is primarily preventable, and prevention is always better than cure. Therefore, the understanding of epidemology, risk factors, clinical features, and management strategies should be at the heart of neurological, psychiatric, nutritional health practices, research, and public health initiatives to effectively tackle this neurological ailment. This approach will cater not only to WKS but will pave the way for dealing with a broad spectrum of diseases arising from nutritional deficiencies.
Thus, the management and prevention of Wernicke-Korsakoff syndrome hinge largely on understanding its complex biochemical background and respecting our bodies’ dietary needs. Embracing a balanced diet rich in thiamin, regular medical check-ups, and careful moderation of alcohol consumption can significantly reduce the incidence of this incapacitating disorder. While the diagnostic and treatment protocols are advancing, these are most effective when implemented early on, emphasizing the importance of prompt recognition of symptoms and risk factors. Lastly, while possible genetic predispositions cannot be modified, being equipped with the knowledge of their existence can certainly empower individuals to take charge of other modifiable factors, enhancing overall well-being and preventing the onset of such neurological afflictions.

Rajan Moonbeam is a dedicated health writer with a Master of Public Health (MPH) degree. Specializing in holistic wellness and preventive care, Rajan combines scientific research with natural approaches to health, offering readers practical advice on living their healthiest life. His work is a beacon for those seeking to navigate the path to well-being with integrity and balance.

